The Significance Of Medical Coding In Revenue Generation
Generation of medical bills and associated revenue are closely linked to medical coding. Both medical billing and coding are involved in the immensely important Revenue Cycle, ensuring that the clinicians and healthcare providers get paid for the services they offer. Let’s take a look how.
Well Begun is Half Done
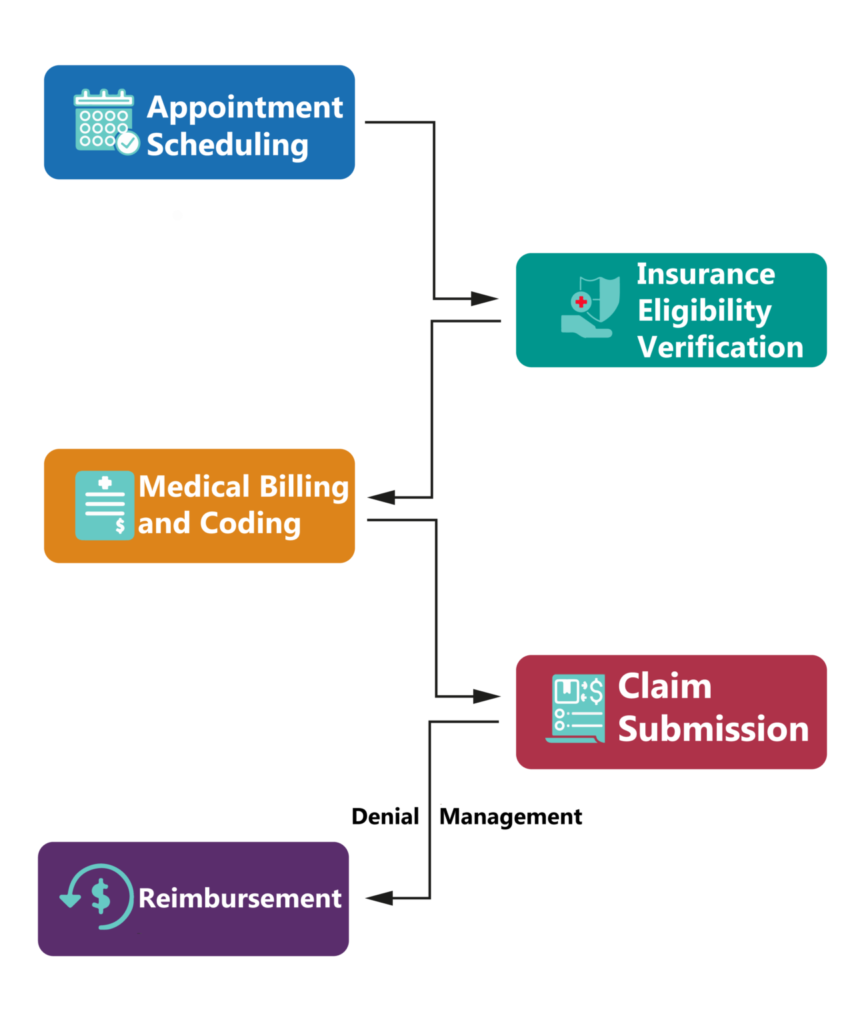
Revenue Cycle Management involves Insurance Eligibility Verification post the clinical visit, Medical Coding, Medical Billing, Claim Submission, and if all goes right, Reimbursement
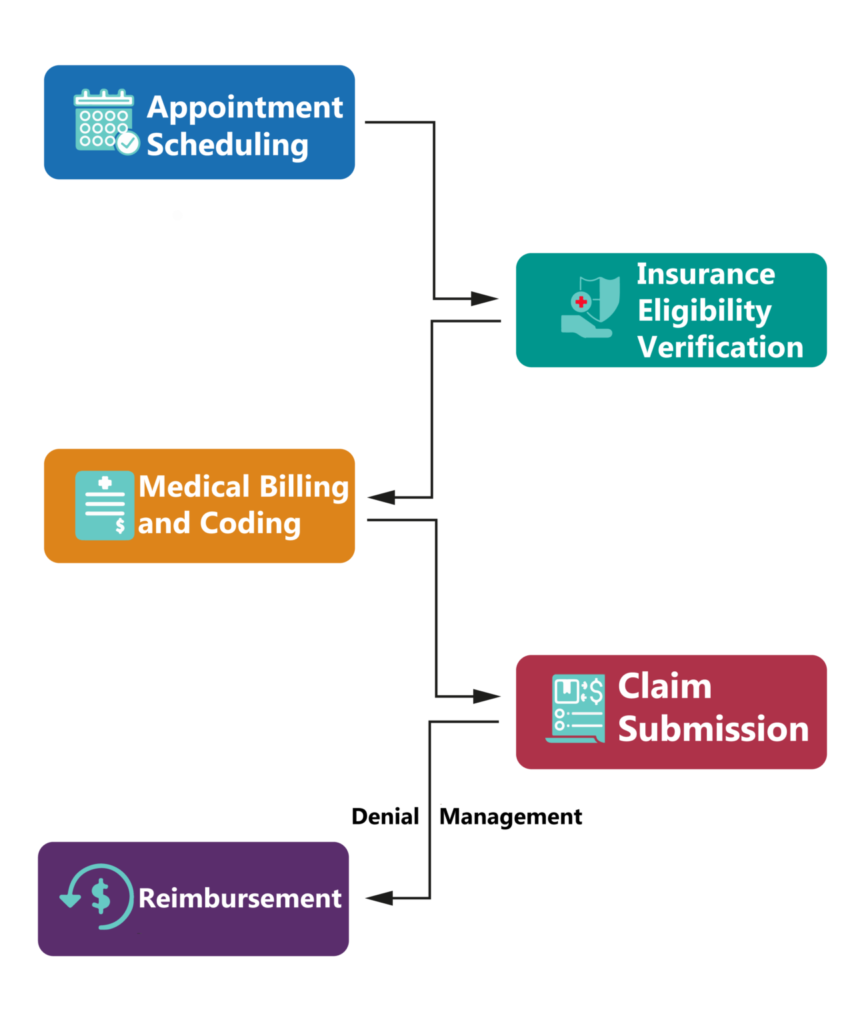
If you follow the cycle closely, you will realize that once the patient’s eligibility for insurance is verified,
medical coding is the first task in the cycle of generating revenue. Hence, any mistake in coding can jeopardize the whole process leading to either delay or loss of income. It is why medical coding becomes the task of utmost importance.
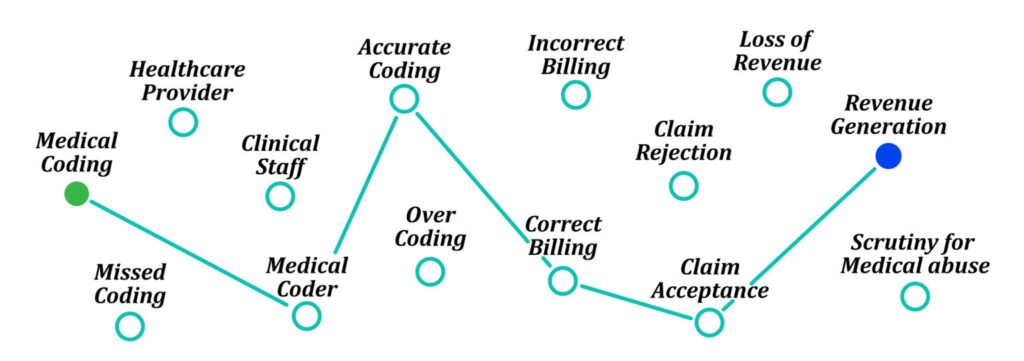
Challenges to Generating Revenue
When it comes to reimbursement and generating revenue, the critical challenges in terms of medical coding present in the form of
- Over Coding or Under Coding – claiming for more than what has been offered or not entirely covering the service by missing entering any of the codes
- Inaccurate Codes – entering wrong codes that do not correspond to the particular diagnosis or treatment
These forms of negligence can lead to
- Claim rejections, delayed reimbursements, loss of partial revenue, and total claim denial
- Federal Penalties, fines, and imprisonment
- Intense scrutiny of your medical practice for medical abuse & fraud
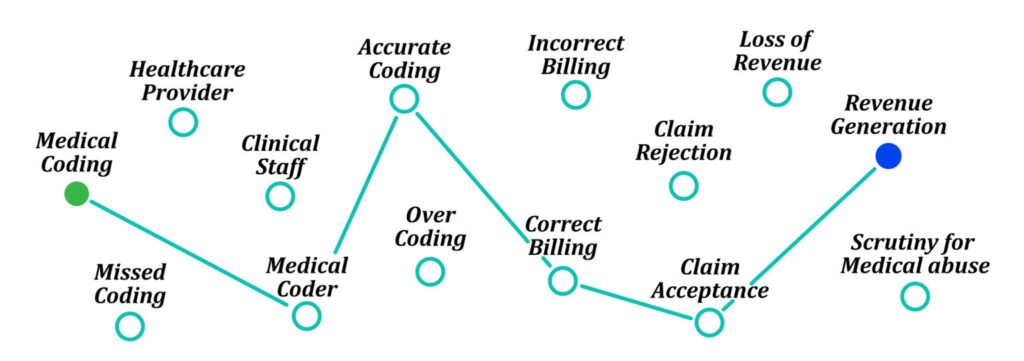
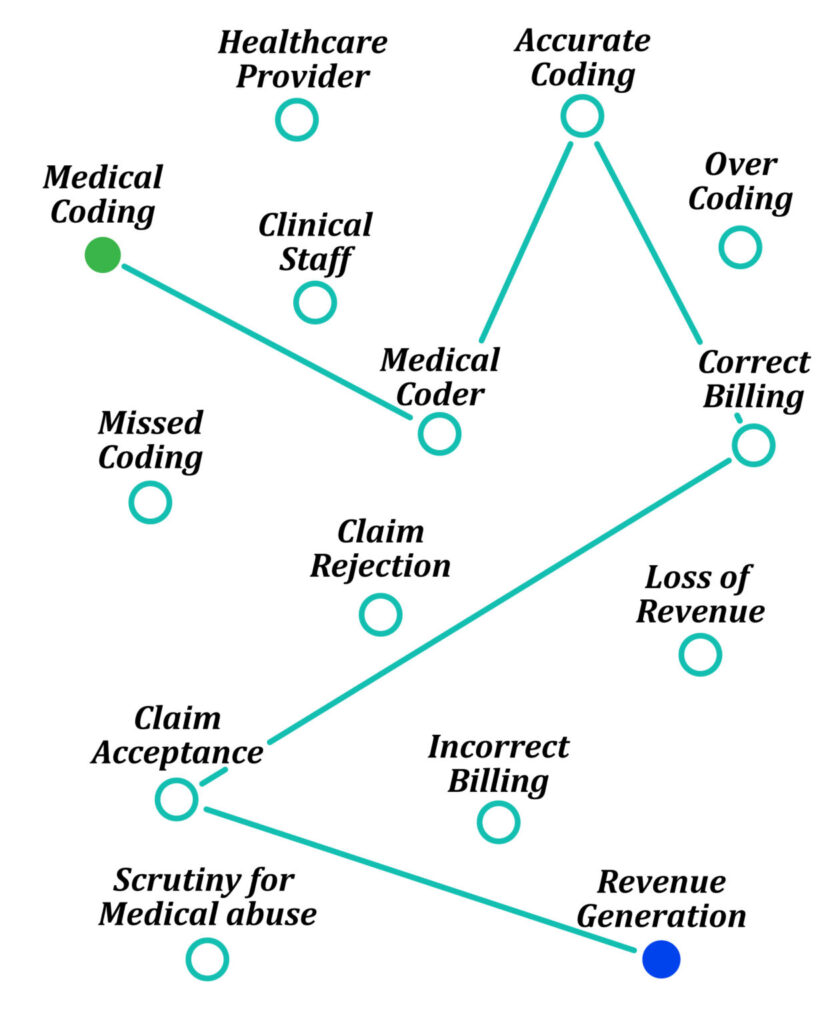
Connecting Dots Between Medical Coding And Revenue Generation
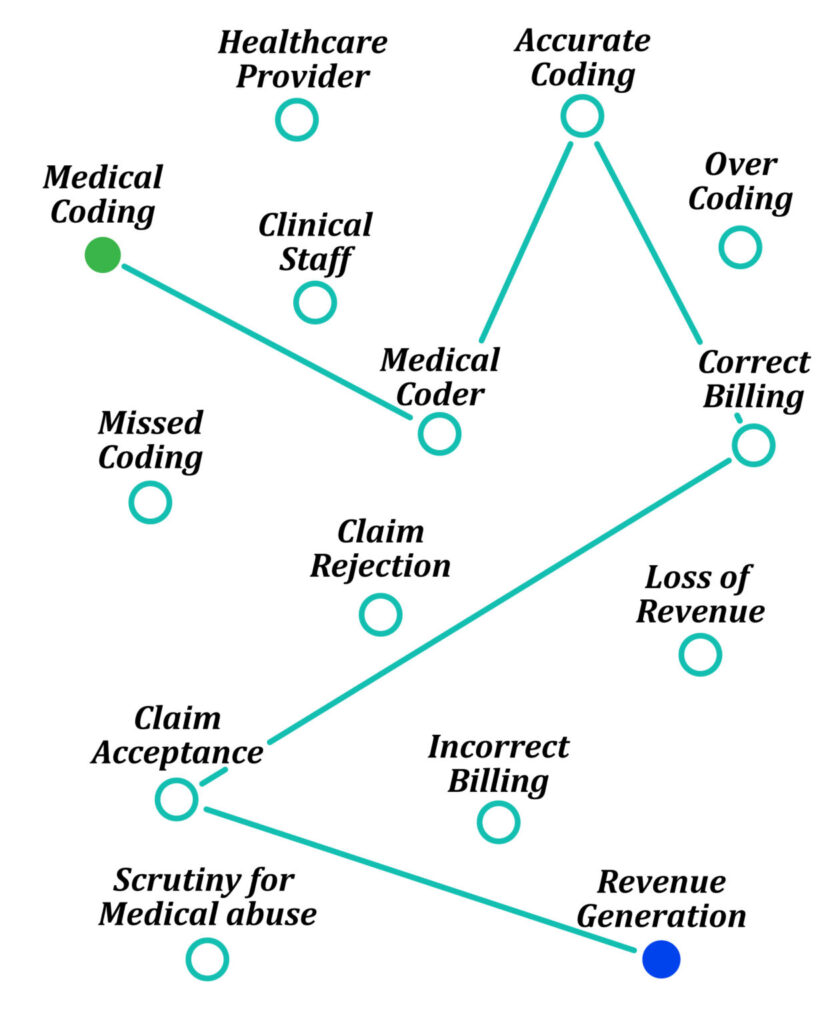
- A well-qualified medical coder identifies medical diagnoses and procedures and documents them into a patient’s medical record, translating them into universally accepted codes, like the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT) codes.
- These medical codes form the basis for medical billing and insurance claims. Insurance companies evaluate the medical document.
- As the expert medical coder performs coding adhering to medical laws and regulations, leading to correct billing, the insurance company accepts the claim.
- Healthcare facilities are then reimbursed for their services depending on the patient’s insurance coverage, leading to revenue generation for both facilities and healthcare providers.
Increased Revenue
Medical coding errors, especially in the treatment procedures, can have implications on the insurance coverage. Correct medical code for the treatment can make a difference between $20 and $2000 in terms of the coverage and revenue.
Eliminate claim rejections
In fact, invalid codes cause most of the denials in the claim submission. Inaccurate medical coding fails to provide a real picture of the patient’s medical history. Accurate medical coding eliminates the scope of claim denials and rejections, thus boosting revenue growth and strengthening the revenue cycle management process.
Streamlining the process
A Medical Coder serves as a significant link in the process of filing insurance by accurately entering the codes and quickly passing the document for billing, thus helping you to streamline the process of submitting the claims to insurance companies.
Remote Medical Coding at service
One does not necessarily have to be present in the facility to perform medical coding. Remote Medical Coders are very well capable of comprehending the medical document prepared during the visit and translating its medical information into universally accepted codes.
The Positive Impact of Outsourcing Medical Coding
No need to hire additional staff
Outsourcing the task of medical coding avoids hiring additional people to the hospital that is already saturated with patients, clinicians, and other nursing staff.
Avoid the financial burden of investing in coders
Companies that offer remote medical coding hire certified Medical Coders and train them accordingly to carry out this responsible task, ensuring compliance, consistency, and accuracy. It implies that the hospital management does not have to invest in hiring or training the coders.
Serves as a cheaper option
A dedicated team of Remote Medical Coders appointed at a particular company will be offering services to multiple facilities as it is their sole job. Therefore, the company will have multiple sources of revenue. Hence, the price that they will charge you for offering the service will be significantly lower than what you would have paid by hiring a couple of Medical Coders in your facility.
Offering Disruptive Medical Coding Services
ScribeEMR has built a highly efficient process to offer robust remote medical coding solutions. The company, which is driven by passionate entrepreneurs, provides its Medical Coders with advanced coding software that accelerates the coding process and ensure more accuracy. Certified Medical Coders have been appointed and trained on various software programs like Epic, CodeLink Pro, AdvancedMD & Flash Code, etc.
ScribeEMR offers coding based on the type of visit & specialty from inpatient and Allergy to Emergency and Urology, covering all the departments. Expert coders are well versed with the latest and revised ICD-10 and CPT 2020 codes, ensuring zero errors in coding and the most accurate billing.
Final Thoughts
Healthcare providers and other hospital staff usually have their hands full with processes and responsibilities involved with the patient care on ground. It is unfair to expect them to carry out medical coding, which is a challenging, lengthy and complex task, without any errors. Therefore, it is best in the interest of both the patients and healthcare providers that the coding is done accurately by a dedicated professional, thus eliminating insurance rejections, boosting revenue growth and strengthening the Revenue Cycle Management.
- These medical codes form the basis for medical billing and insurance claims. Insurance companies evaluate the medical document.
- As the expert medical coder performs coding adhering to medical laws and regulations, leading to correct billing, the insurance company accepts the claim.
- Healthcare facilities are then reimbursed for their services depending on the patient’s insurance coverage, leading to revenue generation for both facilities and healthcare providers.
 If you follow the cycle closely, you will realize that once the patient’s eligibility for insurance is verified, medical coding is the first task in the cycle of generating revenue. Hence, any mistake in coding can jeopardize the whole process leading to either delay or loss of income. It is why medical coding becomes the task of utmost importance.
Challenges to Generating Revenue
When it comes to reimbursement and generating revenue, the critical challenges in terms of medical coding present in the form of
If you follow the cycle closely, you will realize that once the patient’s eligibility for insurance is verified, medical coding is the first task in the cycle of generating revenue. Hence, any mistake in coding can jeopardize the whole process leading to either delay or loss of income. It is why medical coding becomes the task of utmost importance.
Challenges to Generating Revenue
When it comes to reimbursement and generating revenue, the critical challenges in terms of medical coding present in the form of